 A recently published study by Houston Methodist scientists suggests telltale signs of concussions might be found in the gut. By taking blood, stool and saliva samples from 33 Rice University football players, the researchers were able to examine the diagnostic potential of the gut’s microbiome. They say their findings demonstrate that a simple, objective diagnostic test could be developed to track the impact of concussions and signal when it’s safe to return to action.
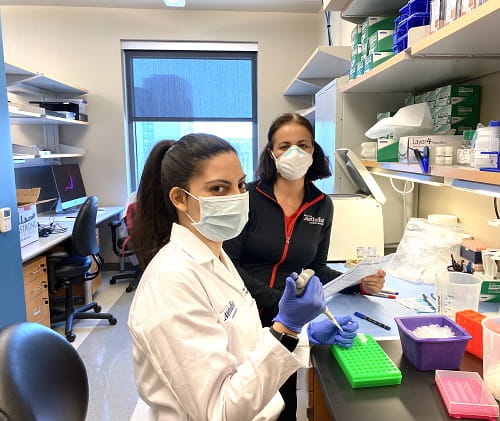
A recently published study by Houston Methodist scientists suggests telltale signs of concussions might be found in the gut. By taking blood, stool and saliva samples from 33 Rice University football players, the researchers were able to examine the diagnostic potential of the gut’s microbiome. They say their findings demonstrate that a simple, objective diagnostic test could be developed to track the impact of concussions and signal when it’s safe to return to action.Drs. Sirena Soriano and Sonia Villapol are part of a research team that showed certain gut bacteria may be used to track the impact of concussions and timeline to recovery.
The findings of this study are described in a paper titled “Alterations to the gut microbiome after sport-related concussion in a collegiate football players cohort: A pilot study” appearing in the May issue of Brain, Behavior, & Immunity – Health, a peer-reviewed journal of the Psychoneuroimmunology Research Society with an emphasis on research that has translational impact and clinical implications. Sonia Villapol, Ph.D., an assistant professor of neurosurgery at the Center for Neuroregeneration in the Houston Methodist Research Institute, is the corresponding author on the study.
While brain movement within the skull may cause injury to nerve cells, such microscopic cellular injuries are not visible on imaging tests like X-rays, CT scans and MRIs, which are more capable of finding injuries on the scale of skull fractures, brain bleeding or swelling. So, the most commonly used test for diagnoses of concussions relies exclusively on self-reported symptoms like blurry vision, dizziness, nausea and headaches, which can be very vague, subjective and often underreported by athletes who want to continue playing. This can make them notoriously difficult to diagnose.
The study, conducted over the course of one season, found a post-concussion drop-off of two bacterial species normally found in abundance in stool samples of healthy individuals. It also found a correlation between traumatic brain injury linked proteins in the blood and one brain injury linked bacterial species in the stool.
While there have been dozens of brain injury biomarkers identified, there has been limited success in developing commercial blood tests sensitive enough to detect tiny increases in biomarker concentrations. However, the central nervous system is also intimately linked to the enteric nervous system, occurring in the intestines, and head trauma invariably leads to changes in the gut microbiota, Villapol said.
After a concussion, the injuries cause inflammation, sending small proteins and molecules circulating through the blood that breach the intestinal barrier and cause changes in the gut, affecting metabolism.
She said these changes in the microbiota could offer an opportunity to acquire a readout of the ongoing injury to the central nervous system.
“Until your gut microbiome has returned to normal, you haven't recovered,” Villapol said. “This is why studying the gut is so useful. It doesn't lie. And that is why there is so much interest in using it for diagnostic purposes.”
While only four of the players in the study were diagnosed with major concussions, the researchers say the results will need to be confirmed in a larger sample size. They also plan to conduct a similar study soon using women’s soccer athletes, who similarly have frequent head trauma.
“Women and men don’t have the same immunities or gut microbiomes, and as a woman and a mother of daughters, I would hate to be that researcher who only looks at men’s issues while overlooking women,” Villapol said. “Women soccer players have very high rates of concussions, as well, and all the same problems when it comes to existing diagnostic methods.”
Villapol’s collaborators on this study were Rice University investigators Kristen Curry, Qi Wang, Michael Nute, Elizabeth Reeves, Sarah Schodrof and Todd Treangen from the computer science and athletics departments; and Houston Methodist colleagues Sirena Soriano, Saeed S. Sadrameli, Rasadul Kabir, Jonathan Wiese, Amber Criswell, Gavin W. Britz, Rajan Gadhia and Kenneth Podell.
This work was supported by the National Institute for Neurological Disorders and Stroke (grant number R21NS106640), Institute of Biosciences and Bioengineering Hamill Innovation Award, National Institute of Allergy and Infectious Diseases (grant number P01AI152999-01) and funds from the Houston Methodist Research Institute. Houston Methodist.
Media Contact: Lisa Merkl
houstonmethodist.org


